Diagnosis Pointers Explained
In the last 17 years, I have been asked a number of times to explain diagnosis pointers. While diagnosis pointers are simple once you understand them, sometimes they are difficult to explain, especially to those outside the claims world. The best way I can think of for now is to put together this diagnosis pointer FAQ. If you have any additions, corrections or would like me to answer other questions, please leave a comment.
What are Diagnosis Pointers?
Diagnosis Pointers are used to describe sometimes complex many to many relationships between submitted diagnosis and service line treatment information on health claims and encounters.
Where did diagnosis pointers come from? Why are diagnosis pointers used?
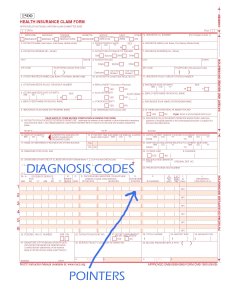
Pointers originated with paper claims. As you can see from the image, there is not a lot of room left in the service line area for diagnosis codes. Instead, the user just enters a number that corresponds with the diagnosis code they are “pointing” to. When EDI started to be used for claims, pointers were a natural fit for two reasons: First, to keep things the same no matter how the data was submitted (electronic or paper) and second to keep EDI “lean”. Transmitting data used to be expensive and charged by the character. Using pointers meant that no diagnosis code ever had to be listed and transmitted more than once.
Why not just list all the Diagnosis at the line?
A properly coded claim often has diagnosis that are not pointed to, but still collected during the encounter. For a service that is somewhat generic like an office visit, the patient may have come in because they had the flu, but ended up getting a full evaluation that showed a previous lower leg amputation and perhaps diabetes management. While the office visit did not address the leg specifically, capturing the diagnosis is still very important.
Are Diagnosis Pointers used in Institutional Claims?
No. Diagnosis pointers are only used in Professional Claims.
Who uses Diagnosis Pointers?
Claims departments use them to determine if they will pay the claim. After loading the pricing for that provider and determining eligibility and coverage, claims decides if the treatment is covered. Among other decisions being made is whether the treatment is covered for the diagnosis. For something simple like an office visit, almost any reason will do, but for something more specific they must match. If the diagnosis is broken toe and the treatment is removed kidney, the claim will not be paid. This is a way to prevent fraud and also a way to avoid paying expensive claims that are really a result of a keying error.
How many diagnosis pointers can there be?
On any given service line there are up to 4. In current EDI (version 5010 of the 837P) the value must be between 1 and 12.
What if more than four (4) diagnosis relate to the treatment?
The coder who is submitting the claim at the provider picks the 4 best and does not point to the others. The idea is to give enough detail / justification for the service being claimed to actually be paid. If one pointer will do, then there is very little reason to point to more codes. In the off chance other diagnosis are relevant to the treatment, they are still available to the examiner at the insurance company who is doing the adjudication – they just are not specifically pointed to.
Why should HEDIS, Medicare Revenue efforts or the new Health Insurance Exchange ignore Diagnosis Pointers?
Pointers are limited to 4 or less per line and average around 1.3 per line. This means that if HEDIS or Revenue only used the codes that were pointed to, codes that are crucial to HEDIS measures or HCC calculations would be dropped. A doctor who did a proper, comprehensive E&M for a patient would almost certainly have the information ignored when processing.
Besides pointers what other limitations are present on Diagnosis Code Submission?
The total number of submittable codes vary by transmission type.
- EDI 837 v4010 Professional: 8
- EDI 837 v5010 Professional: 12
- Current Paper Claim, Professional: 4
- EDI 837 v4010 Institutional: 12
- EDI 837 v5010 Institutional: 25
- Current Paper Claim, Institutional: 18
- ICE (no limit)
Is there any reason Medicare Revenue has to pay attention to pointers?
Certain systems may require them to be submittable data. For example, CMS’s EDPS system that replaces the RAPS system for risk adjustment has them as a required field to be able to submit to the system.
What does it mean when an insurance company asks for numeric diagnosis pointers?
The latest paper form – the CMS 1500 required after April 2014 – has switched from numbers to letters. Meanwhile the EDI (Electronic Data Interchange) files still require a number from 1-12. This puts a small disconnect between the paper data and the electronic. If one were to put a letter into the pointer field of the EDI file, it will reject. Many payers import native EDI or a flattened form of it to put claims into their system. Even if the claim came in as paper, many times it is automatically converted to EDI using OCR / scanning. Done correctly, the OCR vendor should do a crosswalk from Alpha (A-L) to numeric (1-12). This means that if there is an “A” a “1” is put into the EDI field and if there is a “C” a “3” would be sent. Most claims systems will not be updated either so any hand entered claims will have to be converted as well.
The new form can be found here: http://www.cms.gov/Medicare/CMS-Forms/CMS-Forms/Downloads/CMS1500.pdf
Does cross-walking data from a letter pointer to a numeric pointer “change” the data?
Short answer: no. Compliance officers at health plans are often very worried about having a source of truth for the claim. Crosswalks are used throughout data integration projects for a number of reasons. Sometimes it is something as simple as formatting a date from MMDDCCYY to CCYYMMDD. Other times it might be reason codes so that internal codes used in the claims payment process can be understood by those outside by converting them to CARC codes. It is a good idea to document any cross walks or formatting, but the fundamental data has not changed at all.
I work for a MAO and have a performance program around coding (HCCs). We are finding out that we are not getting all the diagnosis codes because the clearing houses are eliminating any code that does not have a pointer assigned to it. Is this industry standard? What have you heard if anything about this? Thanks!
Melissa,
While I have seen it before, it is most certainly NOT an industry standard. There are two reasons that I think are most likely for this, and a host of others if that is not the case:
1. If the Clearing House is not giving you EDI 5010 and instead giving you a file that has been prepared for import into your claim system, sometimes that map is set up in such a way that the diagnosis are stored at a line level in your claim system. Since your claim system stores them at a line level, no more than four would ever be needed on a claim. While your claim system likely has been updated, the map from your clearinghouse may not have been.
2. The Clearinghouse has an older, legacy system that has not been updated and therefore drops codes. I know of one Clearinghouse where this is the case for sure, but don’t want to say their name here on a public forum.
If it is not one of these two, there are a bunch of other things to track down as well that I could walk you through no problem.
Dan
Dan,
How do we confirm that CMS received the diagnoses that were not pointed to? Our clearing house says that they are submitting all of the diagnoses, but we only see the 4 related to the encounter.
Angela,
You asked:
Potentially you are asking two different questions here so I’ll attempt to answer them both.
Q1. How do we know our clearinghouse is not deleting diagnosis before they send information to CMS?
A1. While it is highly unlikely, it is possible. To be SURE, you would need to look at the EDI transaction sent from the clearinghouse to CMS in the “HI” segment of a claim and compare to what you sent them. Also as an ACO you may be submitting to CMS as part of a risk adjusted environment. If that is the case, CMS has reports of what you sent for risk adjustment such as the MAO-004 you can look at.
Q2. Why can’t I see all the diagnosis sent to CMS when I look in my clearinghouse software / interface?
A2. I don’t know. This seems like a bad practice if it is the case. Perhaps there are other more detailed or comprehensive views you could select in their software to see the full claim? This would let you see all the diagnosis for a claim and not just those related to an individual service line on an encounter.
I have an “A” in the Diagnosis Pointer box. What does that mean/
Are you billing for MCR? if so, that A is the new pointer 1 was discontinued for them in 2014
I’m looking at pg 371 of understanding health care. In the diagnosis pointer blocks they have A, B, C and C listed. Have they switched from numbers to letter? I’m looking at the post from Becky, which makes me question this.
I can’t comment on what is in the book, but if they are talking about Diagnosis Pointers, it is wrong.
I can say that if we are talking about transmitting an EDI claim (x12 837P v5010), the standard only allows numeric responses and then only values 1-12. This data is found in the 2400 Loop, SV107.
If we are talking about the paper form (CMS 1500), the Diagnosis Pointers are written / typed in Field 24e. Since people mix this up often, they even wrote on the form that you can only have a value of 1,2,3, or 4. They wrote this with an arrow pointing to 24e inside of Field 21 (Diagnosis).
Hope this helps. If not, let me know and I would be happy to help any way I can.
I believe you write numbers in 24E prior to the new paper form change which began in April 2014, but in the new form you write in letters. Box 21 will now note “relate A-L to service line below (24E)”
Blaire –
Yep – you got it right. Here is a link to the latest form:
Click to access CMS1500.pdf
This means that any payers who use the results of the paper form (accepting print feed, OCR results etc.) will need to do a crosswalk from A-L / 1-12 if they first convert the feed to EDI before loading into their claim system.
I’ll update the post to reflect this.
Dan,
Great article!
I’m currently back-tracking from MA RAPS data to source claim data.
For claims in which there are both MA-valid and MA-invalid procedures, in your opinion, how often are providers billing with pointers vs. simply applying all ICD9s to all CPTs?
Do payers reject claims that don’t have pointing?
Thx-
Josh
Thanks Josh.
When providers submit the information, they can only point to a maximum of 4 Diagnosis codes, so you don’t have to worry about applying all ICD-9s to all CPTs.
Yes. Almost all payers reject claims that don’t have pointers.
For Medicare Advantage risk adjustment though, you don’t have to have a pointer for it to be submittable. Imagine an office visit where a full health assessment was done on a person with many different things wrong. You might have Diabetes, a common cold, a lower leg amputation, a rash of some kind, a headache and a few other things. The only “procedure” for that event was the office visit (say 992.13). The doctor might only point to the cold as the reason for the visit but that doesn’t mean the assessment of all that patient’s health conditions weren’t confirmed or addressed in some way.
Hope this helps.
Thanks, for the quick reply.
So 5010 allows for 12 total Dxs but only 4 per CPT?
Here’s problem: PCP claims with both 992xx and 36415 (Blood Draw) CPTs in which an ICD9 code is pointed to the 36415 only. It’s not common, but it’s not insignificant either. In this case I’m recommending that the 36415-pointed ICD9 not be submitted for RA.
I don’t know if I want to get into specifics of what things should be submitted from a clinical standpoint for risk adjustment here. What I will say is that you should not worry about the pointer at all when working on risk adjustment.
The pointers are there so that when making a claims processing decision, it will cut out some of the noise. You wouldn’t want to pay a claim where the diagnosis was stubbed toe and the treatment was removed kidney right? That doesn’t mean the person didn’t stub their toe. The toe is still stubbed. It was just addressed with a different treatment most likely.
The proper way to code an encounter is to submit all diagnosis for the visit and then for each treatment, submit the most relevant related diagnosis – up to four. More than that, and it just stops adding value for the claims process. That might mean that some diagnosis are NEVER pointed to in a claim. That doesn’t mean the person does not have the condition. It simply means that whoever coded the claim didn’t think the non-pointed to diagnosis were the MOST relevant.
If you don’t like the blood draw because it may have been done by a tech, that is your call – one that is not uncommon. But don’t worry about the pointers when deciding what to submit. Ignore them.
I am being informed that cpt codes can only be filed with 1 diagnosis pointer each as of April of this year. Does anyone know anything about this and where to find the Medicare notice of this change? Please help. Thanks, Gina
Gina,
I have not heard this and a cursory google search didn’t turn up anything. Can you give me any additional background to go on? Who informed you of the change? Maybe I can find something if I know what to go on. The only change I know of in April was the paper form change noted in the article, but that still allows 4 pointers.
I would say that to date, it is good to have multiple pointers. Some treatments are really only done when more than one condition is present and so they are useful to telling the story of what was done and why.
I just learned today of this, and found your blog while looking for some information in relation to it. Section 10.4 of the current version (rev. 3490) of Chapter 26 of the Medicare Claims Processing Manual says (page 16):
“Item 24E – This is a required field.
“Enter the diagnosis code reference number or letter (as appropriate, per form version) as shown in item 21 to relate the date of service and the procedures performed to the primary diagnosis. [Item 21 is the actual list of ICD codes.] ENTER ONLY ONE REFERENCE NUMBER/LETTER PER LINE ITEM. When multiple services are performed, ENTER THE PRIMARY REFERENCE NUMBER/LETTER FOR EACH SERVICE.
“When using form version 08/05, this reference will be either a 1, or a 2, or a 3, or a 4.
“When using form version 02/12, the reference to supply in 24E will be a letter from A-L. Otherwise, the instructions above apply.
“If a situation arises where two or more diagnoses are required for a procedure code (e.g., pap smears), THE PROVIDER SHALL REFERENCE ONLY ONE OF THE DIAGNOSES IN ITEM 21.”
My question is whether this instruction applies ONLY to CMS-1500 claims, or if it applies to CMS-1500 claims and “electronic equivalent”. In other words, will the Medicare Administrative Contractors penalize for submission of (and account for) multiple same-line diagnosis pointers submitted in an ASC X12 V5010 837P transaction?
I’m submitting an itemized bill for an Aflack-style accident policy claim. Unfortunately the person who filled out the form must have been very lazy as they screwed up my health insurance info. They also checked no to “is the patient’s condition a result of an accident,” which puts the validity of my claim in jeopardy. The diagnosis pointer is listed as “AB”. Does this indicate an accident or am I going to have to get a revised bill to indicate an accident?
The “AB” in diagnosis pointer will have no bearing on whether the claim is the result of an accident one way or another.
It is common to forget to check the box on whether the claim is the result of an accident as the default is unchecked in most submissions. I suppose you could try and get the bill revised, but frankly, I would just go up the ladder at your insurance company and not take no for an answer. Talk to their boss and if they say no, talk to their boss’s boss.
We are being told for our Medicare advantage programs we have to send all the diagnosis that pertain to that patient per visit. If the patient has 10 diagnosis codes but only an office visit charge then we can only point to 4 codes. If I send all 10 codes but only use 4 pointers will all the remaining 6 codes be available as long as they are either sent on the HCFA 1500 or the Ansi 837 5010 format?
Rhonda,
You are correct that you would note all 10 diagnosis codes and then only send pointers to the 4 that are most relevant to the visit.
If an office visit takes place where someone came in because they had a cold, but they have lots of other things going on like diabetes, a previous lower leg amputation, a history of AMI, etc. etc. you note all of the things wrong with the person – especially if they were evaluated in any way. You MAO plan will be very happy with the properly coded claim if done this way.
I specialize in a Cranial Prosthesis, would my diagnosis pointer always be the same, like “1” maybe, and opt/hcpcs always the same number? all I do is the Cranial prosthesis.
Sounds like you have one half of the equation done: what was / is done. The pointer is often referring to “why” it is done. Are there many reasons one might do a cranial prosthesis? Say there are many things wrong with the patient – and some are perhaps unrelated to why you are performing the procedure. Use the pointers to indicate what diagnosis are most related to why the procedure is being done. If there are five diagnosis listed on the bill / claim and all are related, you would have four pointers – 1,3,4, 5 for example – and pick the four diagnosis that were the most important / relevant to the procedure.
Let me know if this helps
Hello! I am inquiring about Diagnosis code Pointers – I understand that up to 12 diagnosis codes can be accepted via paper or EDI along with the corresponding diagnosis code pointer on each Service Line. But my question is when we are instructing the providers to bill ALL diagnosis codes which will impact the Risk Adjustment Program (RAPs) and HEDIS for the provider and insurance company – how can a provider bill the pointers for 12 diagnosis codes if they only have say two Service Lines (i.e., 992xx and 364xx)? Some documentation states “the top 4 dx codes” but most provider office personnel will pick the first 4 dx codes which may not include the most important ones. Just wanted to see if there was away to get all of the dx codes for each Service Line.
Thank you, Lee
Hello Lee. Sorry about the delay.
Insurers should ignore the pointers for risk adjustment purposes and consider all claim level diagnosis apply to every line when submitting for risk adjustment – not just those that have been pointed to.
The (up to) four pointers at any line level simply represent the TOP four diagnosis for any given treatment. When coding, you describe a common problem where the FIRST four are used instead of the TOP four. No insurer is going to deny a claim for an office visit for diagnosis reasons and so the provider will be paid and there is no direct, immediate, financial reason to change coding behavior for the coder / submitter.
I have seen problems deep within large insurers systems (claim systems, data warehouses, risk adjustment platforms, EDI Mapping tools etc.) where only pointed to Diagnosis are written out. This represents a data DROP and needs to be fixed as soon as possible.
Thanks for the information. Hopefully in the ACS X12 6020 version (which I haven’t seen, yet) the industry will address this issue. Thanks for your help.
Hi Dan . . . How is a ‘data drop’ addressed after the claim has been processed and paid? Is there a way to resubmit the additional diagnoses for HCC capture only without re-processing of the claim? Thanks in advance for any help.
Thank you,
Kathy
Kathy,
The most common ways data drops are resubmitted are via a chart review. There is a specific way to format the EDI submission to reflect the fact that a chart review has been completed and the data is not an original submission.
Chart reviews are very common in risk adjusted environments.
Dan
Hi, Are the diagnosis code pointers keyed in by the billing person at the provider’s office when sending a claim? This is confusing, as I don’t know if the box is filled in automatically, or if we are supposed to fill it in. Thanks for your help.
Howdy Tish.
Usually the diagnosis pointers are entered by the biller at the provider’s office. I suppose it is possible that some applications default diagnosis pointers in some systems. Also, instead of entering a pointer, the biller might click on or select in some way the diagnosis that should be pointed to on a line.
Hi! I had a question I hoped you might be able to shed some light on. We’re having trouble with our multiple immunization claims passing the edits of our clearinghouse since the change to ICD 10. They have simplified the diagnosis for all vaccines down to just one code, Z23. We routinely give 4 vaccines in a single visit, plus the administration/counseling CPT codes. On each claim we’ve tried to submit, it gets rejected as “diagnosis codes must be unique”. I have contacted the clearinghouse (can’t give billing advice) and searched everywhere for the answer to this dilemma. All that I can find is that this should be so much simpler, since each vaccine doesn’t have a separate diagnosis any more. Any advice?
Without knowing everything, the two most likely possibilities are:
The clearinghouse is incorrectly rejecting the claim. Perhaps something in their logic that was updated for ICD-10 has broken this as well. While it is possible that you could convince the clearinghouse to look into it and provide a better explanation, I would also contact the health plan and have them work it from their end since the clearinghouse is enforcing (incorrectly in this case) the plans edits and therefore should have more influence over how their edits are enforced. Have the plan supply to you the exact logic that is supposed to be followed. If this is a covered service, they need to accept your claims and the responsibility should fall to them to get it resolved in short order.
While there are other possibilities, I don’t think I have enough information to come up with anything else. As a personal favor, please reply with an update to what the resolution is to help satisfy the professional curiosity that fuels this post in general. Or feel free to reply with any other details that you think might help me troubleshoot further.
Thank you for getting back to me! I’m implementing your suggestions and waiting to see what results. I’ll keep you posted on what I find out. I’d love to know if we are the only ones having trouble with this, if this is a common problem among pediatric offices (since we routinely give multiple shots at a time). Thanks again!
My pleasure! Very happy to help. Please let me know what ends up being the issue (#1, #2 or something else) so I can help others if something similar comes up again.
I am a PT. I do my own billing, which is very mostly Medicare. I attended a Medicare seminar years ago, in which we were given a book which allowed us to choose appropriate diagnosis pointers for each diagnosis using ICD9 codes, which correlated to the procedure code. Now that we use ICD10, I am not sure how to choose the appropriate diagnosis pointer for each procedure code. Any help would be most appreciated. Thank you!
Howdy Joan. Any way that the article itself helped?
I’ll give a few ideas to you, but please let me know if you have more specific questions.
You can still point to between 1 and 4 codes for each procedure. So even though the codes are different, the pointers should still work the same way for you.
If before you had two ICD-9 codes related to a single procedure and now you have four ICD-10 codes related to a single procedure, instead of using pointers 1,2 you would use pointers, 1,2,3,4 to relate them. If that is unclear or doesn’t help you specific question let me know. In fact, if it DOES help, kindly let me know that as well as I am always pleased to either hear that I helped, or learn how I could answer questions better.
Hi Dan! Thank you for posting this useful page. I am a medical biller in a chiropractic office. With the implementation of the new ICD-10 codes, our level of specificity has greatly increased. In ICD-9, we simply indicated that an adjustment was done in a spinal region, in ICD-10 we must also specify the level (ex. Thoracic level T1/T2, T4/T5, T7/T8 etc). So there are times where the codes for one area take up the first four. Our contracts pay out depending on how many “areas” we adjust. So we commonly use one of three CPT codes, 98940 1-2 areas, 98941 2-3 areas, or 98942 3-4 areas.
I have been having some trouble with injury payers denying saying that we are not pointing to enough areas to support diagnosis for how many areas we are billing for. They recommend that we switch our pointers in box 24E to indicate A-L instead of A-D. However, the resources I have consulted state that we can only point to ABCD. Also, our software system only allows us to manually point to A-D, I literally cannot choose more codes to point to unless I set it to “use dx list from chart,” which frequently does not reflect the correct number of areas with just the first four codes.
I know that some of these issues may need to be individually reconciled with the payers and our software company, but I am hoping that you can advise me on the box 24E dilemma in a few ways. First, is it okay to point to 4 dx codes that are “out of order” from the dx list provided by the doctor? For example, if he inputs 4 thoracic dx codes then 3 lumbar then 1 for sacrum, is it okay to select any of the 4 of the 7 codes to point to in order to indicate to payers the number of areas adjusted? This would mean only these four codes would show up on our hcfa and not the full 12+ that the doctor reported in his chart note.
Second, do you know if it is appropriate to change the pointer from A-D to A-L? I am slightly confused because I’ve heard a lot about it but many sources still say regardless of A-L we can only point to four codes… is it common for providers to switch to A-L?
Thank you!!!
Courtney,
The clear thing here is that your software vendor is NOT ICD-10 compliant if they don’t allow enough pointers to get to any of the 12 potential codes. You need to fire the vendor, get a refund, get the software upgraded if there is a new one or get a typewriter to fill these out manually (last one being a really bad idea in case that is not clear). Have the vendor call me if they say otherwise.
As far as the rest is concerned:
You can list up to 12 ICD-9 / ICD-10 codes
You can point to up to 4 ICD-9 / ICD-10 codes for any given service line
Any of the 12 codes can be pointed to in any order
– eg ABC, ACEG, BLD, CBA etc.
The order should generally be the most relevant Diagnosis code for the procedure being billed is pointed to first with the others being pointed to in descending order. The first code pointed to is generally considered the primary reason for the treatment.
Please tell me if this helps either way and if you have other questions I didn’t make clear.
Hi Dan excellent forum to get questions answered!! Thank you! I was wondering in the 2nd part of Courtneys question above you didnt mention if it was in fact acceptable to indicate A-L in 24E?? As with the very specific dx codes now needed for chiropractors and if 4 areas are adjusted that may require using all 12 dx codes indicated to justify getting the 4 area CPT code paid tbus indicating A-L OR should i just pick one subluxation code for each area being adjusted to point to in random order as u previously mentioned was ok?? Also my other concern is that the secondary or supportive dx codes i am told may help justify getting the maximum # of visits alowed paid so being forced to leave out the supportive codes bec i have to indicate 4 subluxation codes already may result in not getting the max # of visits paid?? HELP ME DAN lol
Hi Dan excellent forum to get questions answered!! Thank you! I was wondering in the 2nd part of Courtneys question above you didnt mention if it was in fact acceptable to indicate A-L in 24E?? As with the very specific dx codes now needed for chiropractors and if 4 areas are adjusted that may require using all 12 dx codes indicated to justify getting the 4 area CPT code paid tbus indicating A-L OR should i just pick one subluxation code for each area being adjusted to point to in random order as u previously mentioned was ok?? Also my other concern is that the secondary or supportive dx codes i am told may help justify getting the maximum # of visits alowed paid so being forced to leave out the supportive codes bec i have to indicate 4 subluxation codes already may result in not getting the max # of visits paid?? HELP ME DAN lol
i forgot to check to please notify me of any new posts or comments via my email at bodydoc9@aol.com
Gina,
Yes you can use A-L in 24E
The order of the codes is not random. For each encounter, you can list up to 12 DX codes. These codes may or may not all be pointed to. For one procedure, point first to the primary reason (DX code) you are performing the procedure. Next point to any other reasons you may be doing the procedure, up to three additional codes.
As far as getting paid, as a general rule, more detail helps. So even if you never point to some of the codes, include at the encounter level as many as are relevant to the encounter. Also, be sure to point to as many (up to four) that are relevant to the procedure in the order of importance. If there are leftover DX codes that are relevant, but not pointed to, at least the payer has them at the encounter level and can see them there. Just because a code is not pointed to (because you already used four) doesn’t mean it is not relevant to the procedure.
Let me know if this helps.
Dan
Hi Dan:
this is my first time using the CMS1500 VERSION 2/12., my Main Problem is with field 21 and 24E.
in field 21 — must I fill all the line from A to L with a diagnose or just the first four . and how is this field connected to 24E– what should I type in field 24E.
please help me to understand this.
Looking for primary diagnosist which this person alot going give me answer here here are diabete Mellitus, hypertension benign,
If the dictation is giving more than 4 codes, is the coder requiered to use upbto 12 codes per line? Or do they have to codebonly the 4 more important ones?
Yazmin,
Pretty sure the FAQ covers this already, but diagnosis codes are not at a service line level. Only the pointers are. You can point to up to 4 that you think are most relevant.
You should put every code (up to 12) from the “dictation” at field 21.
Thank you very much Dan.
Hi Dan ,
I am having an issue with paper 1500 that are being mailed to a Risk Plan. The office is putting all MRA codes on the claim however it seems the plan is only using the 4 that are pointed to in 24E with the E&M CPT. We have been told the claims are “hand keyed” by the plan when they receive the “paper claims”. Have you run into this before ? I was told I can repeat CPT to the paper claim with and continue down the alphabet until I have covered all of my DX. Have you heard of this or dealt with this before ?
Yes. Usually it is because they are scanned and hand keyed off shore. When they key the information in, it could be that their vendor’s entry process only has four places to put codes because they have not updated their process to take more codes.
Either way, if anyone at the plan in management understood that they were dropping codes due to their process, they would be very upset.
Hi! Our clearinghouse continually spits back claims that fall under the following criteria:
More than four ( >4 )- let’s say we have 7 different diagnosis codes on the claim itself (all the issues the patient is complaining of or still uncontrolled);
And, then four (4) of those 7 diagnosis codes are “pointed” to the office visit (cpt 99204)… and that’s it. No other procedure performed. Just that office visit for a patient with a plethora of medical issues– that are all duly and thoroughly addressed by the health care provider.
Now that we are ready to “bill” the claim out, my electronic clearinghouse claim 837 still enables me to list up to twelve 12 different diagnosis codes for this patient’s one service date, but if I only point to 4 of them (only because we are imposed a limitation of up to 4 diagnosis codes per line charge that can be pointed to), and send it out, the rejections come back because I did not “Point” to all 7 of them…I am confounded by this, and frankly- not all patients have just 4 things wrong with them. Some have, dare I say, 5…. or 6….. So it appears that our coders are to use their own best judgement and just delete out all but the 4 diagnosis codes on that respective claim that we would then “point” to for that office visit charge, correct? Please help. This is causing delayed claim submittals, and double the work for our A/R reps. Thanking you in advance!
Howdy Diana! What you described is very clearly wrong. If you only have one service line, you can’t possibly point to all 7 codes.
My advice is to get help. The payer doesn’t want you to get rid of the codes to make it submitable and would be very mad at the clearinghouse if they did. If you can’t get anyone knowledgeable at the clearinghouse to help, call your payer and get beyond the first level of customer service until you get to someone who understands what you are telling them.
What is the name of the clearinghouse you are working with?
Hi Dan, Thanks so much for your reply. Our clearinghouse: Trizetto (formerly Gateway EDI).
The issue has been brought to the attention of my superiors, and we need to have this rectified STAT…Would you be able to advise or assist any further?
Regarding the above question from Diana.
I come across this exact scenario on a daily basis in our medical office. Dan – can you point me to the literature where it talks about the # of diagnosis and CPT pointer you reference. My boss fails to grasp the fact that even though there is only 1 CPT code and perhaps 7, 8 or 9 Dx codes that we should only be putting 4 Dx codes per 1 CPT code and remove the additional 7,8 or 9 diagnosis codes even though we only have 1 CPT code.
Thank you.
You are not removing any of them. If there is one treatment (an office visit let’s say) and there are 9 things (diagnosis) that were evaluated, confirmed, diagnosed or related in any way during that visit, you list them all in the diagnosis section.
Then when you are at the line level, you point to the ones that are most related to the visit. . . up to a maximum of four.
Dan,
I hope you will answer the question posted by Gregg Bingham on May 23, 2016. It appears as a reply to an older post by you on August 23, 2014.
Dan notes, as I have, too, that Medicare instructions for CMS-1500 claims state that one should use only one diagnosis pointer for each service, i.e., for each claim line or each CPT code.
Dan continues: “My question is whether this instruction applies ONLY to CMS-1500 claims, or if it applies to CMS-1500 claims and ‘electronic equivalent’. In other words, will the Medicare Administrative Contractors penalize for submission of (and account for) multiple same-line diagnosis pointers submitted in an ASC X12 V5010 837P transaction?”
Furthermore, I am wondering whether, if Medicare will accept more than one diagnosis pointer for a CPT code when the claim is submitted electronically, it might be to the provider’s advantage to list more than one when appropriate, as it might be a step in the direction of justifying a higher-level E/M code.
Use as many as are relevant starting with the most directly related reason (Diagnosis) to the least up to a maximum of four. I suppose more is better if they are all relevant.
Correction: I should have written “Gregg notes” and “Gregg continues” in my post above. I wrote Dan instead of Gregg. Sorry for the confusion.
Dan, I’m a Massage therapist and have a family that is Authorized by Aetna “Foreign Service Benefit Plan” to get massages. I’ve been trying to get this paid through electronic, but the reject due to: 2 # errors LC1701 – Diagnosis Code 1(A) is Invalid. I’m using ICD-10 code 8E0KX1Z.
Any suggestions or direction, greatly appreciated.
Al
Hello, I have two diagnosis codes . So it would be “A” which is “1”. And “B” which is “2”. So in 24e what would I put ? Would I put 12 ?
The last two sections of the FAQ as well as numerous questions / responses speak to this. Please read it over and let me know if you still have questions.
Where can I find the descriptions of A-L? I am billing medical for a dental problem and can’t seem to find out which diagnosis pointer to use.
Julie,
I believe this has been answered in the article. Please re-read it and let me know if it is still not clear or you can be more specific about what is still remaining.
Dan
WHAT DOES A OR 1 MEAN? 1-12,A-L. I’M LOOKING FOR A LIST THAT SHOWS WHAT THE LETTERS STAND FOR.
Sorry you are having a tough time with this. Please try and take a look at the article from the beginning and see if it helps. I DON’T THINK THE CAPITAL LETTERS ARE HELPING ME UNDERSTAND WHAT ISN’T CLEAR . . . ahem.
Thank you, I finally figured out.The diagnosis pointer in 24 E relate to box 21 A etc. I did not mean anything by using capital letters. Sorry.
I have 4 diagnoses for a 99213 visit and our billing system only allows space for 2 letters for the diagnosis pointer. How do I get it to indicate ABCD?
My guess is that your billing system is electronic right – not paper? So it SHOULD be looking for numbers not letters. The two digits are there because each pointer can be up to two characters (1-12). See what happens if you enter a “1” or a “01”. Perhaps it then allows you to enter another pointer?
I have a claim with 6 diagnosis codes billed. One code was invalid when file . Is it a CMS requirement to deny the whole claim if the only one code is invalid however said code only points to line 2 of the claim? If so would you know where I can find the information in writing on this ?
Not sure specifically on the CMS side, but I would guess that any invalid diagnosis codes makes the whole claim denied at most plans. Diagnosis are submitted on the claim level whereas treatments are submitted on the line level. So some plans may only reject a single line and allow the rest if there is a problem with a treatment, but likely won’t be able to do the same with a diagnosis. Rather than find in writing where this might be, just to get a similar answer, I would suggest it be refiled instead with valid diagnosis codes.
Hi Dan,
Thank you for sharing this helpful article. I have a question regarding EDPS Submission for an MA org.
We are getting Error 254- Principal Diagnosis code is invalid for DOS and Error 255- Diagnosis code is invalid for DOS on some of our claims.
How can we resubmit the Claims for which we received 254-255 errors? Can we remove the Diagnosis which is either a duplicate or expired for the DOS? If we remove those Diagnosis from the header then what do we need to change at the details level as far as Diagnosis pointer is concern?
for example
HEADER
ICD_1 ICD_2 ICD_3 ICD_4 ICD_5 ICD_6 ICD_7 ICD_8 ICD_9 ICD_10 ICD_11
E782 F3WRNG F410 J309 I059 I369 R5381 R5383 R0989 K5730 Z6830
DETAIL
LINE_NUMBER SERVICE_CODE_QUALIFIER SERVICE_CODE DIAGNOSIS_IDX
1 HC 99213 2134
2 HC G8419 B
3 HC 3074F 1234
4 HC 3078F 1234
If we were to remove ICD_2 (F3WRNG) , how would it effect the Detail Diagnosis_IDX column?
Peter,
Feel free to give me a call and we can discuss. This is a pretty specific scenario and I have enough questions that attempting to answer it here without other information wouldn’t work.
Dan
Hi Dan,
Thank you for your article! I am a billing supervisor and have been going back and forth with a vendor stating that we can only bill 4 diagnosis per claim. They also stated it was a CMS guidelines. Well I know this is simply not true and I can’t get anywhere with this software or get the practice doctors to understand that the software that we are using is not compliant! Help! is there a formal complaint that I could do. I have been complaining for over a year!
Drina
We can hope they are not incompetent and instead count on confusion here perhaps? We can only link 4 diagnosis per service line, but that is in NO WAY TRUE for the claim. A professional claim can have up to 12 diagnosis. Send them a copy of the paper form with the 12 spaces for diagnosis circled as proof perhaps?
Hello Dan!
There are certain procedure codes that must be grouped together for billing purposes. The claim may get denied by the payer if the procedure codes are sent in different claims. One of the examples might be that the patient showed up for Office Visit (99202) and after further counseling, ended up receiving a Depo-Provera shot (J1050). Now, you cannot receive a shot without having an encounter with a clinician, so to speak these two services should be grouped together into one claim.
In this scenario, suppose that the clinician documented 15 diagnosis codes. If we are to send 12 diagnosis codes per claim –
1) Should we split the claim into two so that one claim contains 12 diagnosis codes and the other claim contains 3 diagnosis codes? If we go this way, it may affect adjudication of the claim.
2) Should we keep the single claim with 12 diagnosis codes, and omit the remaining 3 diagnosis codes? If we go this way, it may affect the accuracy of reporting (e.g., for HEDIS measures).
Best wishes and please keep doing the great job of disseminating knowledge! Regards – SK.
To be precise –
1) Should we split the claim into two so that one claim contains 99202 with 12 diagnosis codes and the other claim contains J1050 with 3 diagnosis codes? If we go this way, it may affect adjudication of the claim.
2) Should we keep the single claim with both 99202 and J1050 along with 12 diagnosis codes, and omit the remaining 3 diagnosis codes? If we go this way, it may affect the accuracy of reporting (e.g., for HEDIS measures).
Are there 15 total codes or do three overlap? If so, send one claim and for each line, point to the four most relevant codes. But it sounds like you already would have figured that out.
I am not a billing expert although I spend a lot of time “billing adjacent” as an EDI expert. I am especially weak on clinical. That said, for HEDIS I would imagine the condition codes are less treatment specific than you might imagine. So if someone has been diagnosed with a broken toe one day and another day are evaluated for their diabetes, that patient is a patient who had both a broken toe and diabetes in the same calendar year – even if they didn’t come in on the same claim.
The person seeing the patient to administer the Depo shot in most cases hasn’t evaluated the patient for the other conditions so should just be putting down the ones relevant to the shot. Just like the endocrinologist isn’t an orthpedist (broken toe / diabetes).
Not sure if this helps.